Epicardial fat masquerading as hemopericardium in a post PCI patient
Dr Himanshu Gul Mirani
Nottingham University Hospital, NHS Trust
Case Presentation:
An 80-year-old female presented to the emergency department (ED) with complaints of acute chest pain and dyspnoea, 2 days post primary percutaneous intervention (PCI) for ST elevation myocardial infarction (STEMI). She was haemodynamically stable, needing two litres of oxygen via nasal cannula. Electrocardiogram showed post MI changes, with no acute STEMI and was Sgarbosa criteria negative.
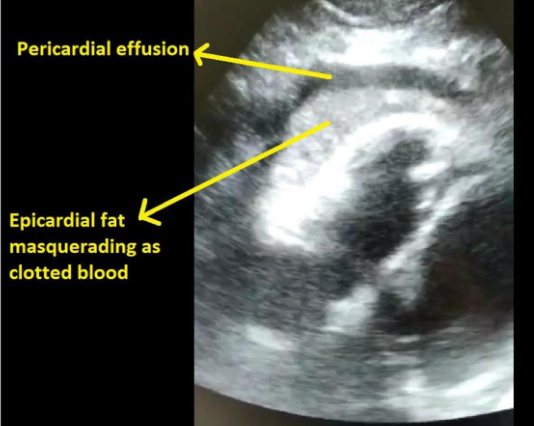
Bedside ECHO showed an echogenic lesion around the right ventricle with a surrounding rim of pericardial fluid. In the context of recent STEMI and PCI, concerns were raised if this was hemopericardium secondary to myocardial rupture or coronary vessel injury from the recent procedure.
Subcostal view of the heart showing the epicardial fat and pericardial effusion
Management and Outcome:
The patient had a CT aortogram which confirmed there was no acute aortic syndrome or ventricular
rupture. Patient had a formal ECHO in the ED by the cardiologist and the lesion was reported to be epicardial fat.
Key Learnings and Points:
Epicardial fat is a common finding. Its thickness is a marker of cardiovascular risk and has been associated with insulin resistance, atherosclerosis, metabolic syndrome, and coronary artery disease. It can be confused with hemopericardium or pericardial effusion. Features suggestive of epicardial fat are that it is usually found around the ventricles and is less likely to be seen around the atria or be circumferential around the heart. Epicardial fat is adherent to the outer wall of the myocardium and moves with it during cardiac cycle. It is not associated with tamponade physiology or dilated inferior vena cava. In this case the associated small rim of pericardial effusion was thought to be secondary to the recent MI.
